If your dentist prescribes a root canal, then you’re probably wondering what a root canal is — or if you do know, maybe you’re nervous about the procedure. No need to worry, though, because root canals are a safe and common procedure performed millions of times every year. According to the American Association of Endodontics , root canals are as routine as getting a filling, relatively painless, and extremely effective as treatment for a damaged or infected tooth. So what exactly is a root canal?
A root canal is a procedure, typically performed by an endodontist , to repair a damaged or infected tooth while still preserving the remaining healthy parts of the tooth. To perform the procedure, the damaged or infected tooth is left in place within the gum line while an endodontist thoroughly cleans the canal surrounding the tooth’s roots.
Why You May Need a Root Canal
You may need a root canal if you have a damaged or infected tooth that affects the dental pulp of the tooth. Dental pulp is the soft core at the center of a tooth that extends from the crown of the tooth (the visible top part) down to the tip of the roots deep within the gumline and extending to the jawbone. This dental pulp contains nerves, blood vessels and connective tissue, so when a tooth becomes damaged (by cracking or by cavity), bacteria can enter and damage the tooth’s health.
If this bacteria or decaying material is left untreated within the tooth, you run the risk of getting an infection or having a tooth abscess manifest. These symptoms can lead to pulp death, bone loss and a full loss of the tooth itself. Other symptoms that may indicate a need for a root canal are swelling around the face and neck, holes in the tooth (which cause toothaches, tooth pain and temperature sensitivity) or even gum swelling.
Getting Started on Root Canal Treatment
A dentist or endodontist (“endo” being the Greek word for “inside” and “odont” meaning “tooth”) typically performs root canals. Once they take dental X-rays to assess the damage to the tooth, they will administer a local anesthetic to the affected area to help suppress any feeling. To keep the tooth clean and dry during the procedure, dental specialists use a small, rubberlike sheet called a dental dam in the mouth.
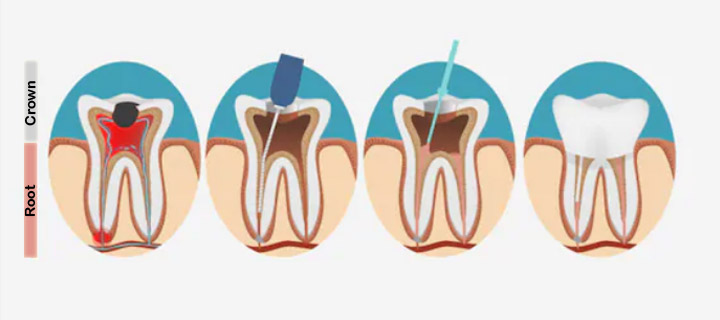
During the procedure, your dentist or endodontist will remove decay from the outer areas and then make an opening through the crown of the tooth. This is done so that the dentist or endodontist can access the dental pulp inside. Once the hole is made, the infected or diseased pulp is removed from the tooth.
Clearing the Root Canal of Infection
Once the dental professional removes the diseased or infected pulp, they flush and clean the pulp chamber and root canals. If necessary, they may reshape or enlarge the root canals to allow for better access for the filling process that comes later.
After a thorough cleaning, your dentist or endodontist may apply medication to the pulp chamber or the root canal to help clear any lingering infection they may have missed. If the original infection has spread to other areas of the mouth, you may get a prescription for antibiotics or have another procedure scheduled, depending on your dentist’s recommendation.
If your root canal procedure requires more than one visit, your dental provider may give you a temporary filling for the crown on top of the affected tooth. This temporary crown helps protect the tooth from food debris and saliva while you wait for your next procedure. While this crown remains in place, avoid biting or chewing with it until the full tooth has been both treated and restored to your dentist’s satisfaction.
Filling the Root Canals
Once the tooth has been properly cleaned and treated, it’s time to refill the tooth to restore its structural integrity. It’s possible that more anesthesia might not be needed for this part of the process. If you had a temporary crown and filling placed on the tooth, your dentist or endodontist will remove and replace with a compound of rubber and sealer paste that will fill the remaining area inside the tooth. Once the dental pulp area is refilled with this paste, they will add an adhesive filling to the root canals to make sure they’re protected from saliva or food debris.
Final Stage of Root Canal
By now, your dentist or endodontist has drilled into your tooth, hollowed it out, thoroughly cleaned it, and then refilled it with sealant and adhesive paste. Now the dentist must restore the tooth’s strength to protect it from future damage and allow it to be used normally again.
This starts by placing a crown on top. Crowns are made of several different kinds of material, most notably gold or porcelain fused to metal, but they can also be made of porcelain alone and can be tinted or colored to match the exact color of your other teeth so they don’t stand out.
Your dentist or endodontist may also recommend inserting a metal post into the tooth for added structural integrity before the crown is applied.
After Your Root Canal
Your tooth, and the surrounding area, may be a little sensitive for a few days after the procedure. This is completely normal, and over-the-counter pain medications can help alleviate any lingering pain or pressure you may experience. If the pain continues for longer than a day or two, you should contact your dentist or endodontist immediately for further recommendations.
Otherwise, your restored tooth and crown should be both functional and aesthetically pleasing. Practicing good and constant oral hygiene will ensure that your restored tooth will continue to work well for a lifetime.
Ask your dentist or endodontist if you may need a root canal in the near future or if there’s anything you can do to help prevent it.
